All Issues
Cognitive and motivational factors support health literacy and acquisition of new health information in later life
Publication Information
California Agriculture 64(4):189-194. https://doi.org/10.3733/ca.v064n04p189
Published October 01, 2010
Abstract
Health literacy refers to the ability to read, understand and use health information to maintain or improve one's health. Health literacy skills have been linked to outcomes such as medication adherence, improved health and decreased health-care costs. Health literacy is particularly low among older adults. Given demographic projections that 20% of the U.S. population will be over age 65 by 2030, there is a pressing need to understand health literacy in later life. We present such a framework, as well as data from two studies that show how cognitive and motivational factors support one aspect of health literacy, namely, the acquisition of new health information. A clearer understanding of these issues will provide insight for targeting educational interventions designed to increase health literacy among aging adults.
Full text
Health literacy refers to the ability to obtain, process and understand the basic information and services needed to make appropriate decisions regarding one's health (Institute of Medicine 2004). The American Medical Association defines health literacy similarly, as “the constellation of skills, including the ability to perform basic reading and numeracy tasks, required to function in the health-care environment.”
Health literacy is needed to understand medical information and instructions, communicate effectively with health professionals and manage one's own medical treatment.
In general, “health literacy” includes a broad range of skills including the ability to understand language well enough to accurately complete medical forms, comprehend spoken and written medical instructions, and communicate symptoms and concerns to medical professionals, as well as the ability to seek and understand information regarding illness and treatment options outside of the medical establishment. Individuals with low health-literacy levels may be less likely to receive adequate health care because they avoid or delay seeking care. In cases where they do seek help, they are less able to benefit due to comprehension problems during and after the care visit. Furthermore, they are less able to regulate the treatment of their chronic diseases, less likely to adhere to medication regimes and more likely to visit emergency rooms (Murray et al. 2004; Schillinger et al. 2002). Not surprisingly, low health literacy has been associated with increased health costs (Marwick 1997).
Low health literacy may be more prevalent than many realize. Among English-speaking patients, researchers found that more than 30% could not comprehend basic health materials, 25% could not accurately read appointment slips and 40% could not understand their prescription labels (Williams et al. 1995). The White House Office of Management and Budget estimated that language barriers affect some 66 million patients annually (Newman 2003). Moreover, older adults are more likely to have problems related to health literacy than younger adults (Rudd et al. 2004). One estimate suggests that 30% to 40% of English-speaking older adults are unable to comprehend written health-care information (Benson and Forman 2002; Gazmararian et al. 1999). In fact, one study found that 2,512 community-dwelling older adults with limited health literacy were nearly twice as likely to die in a 5-year period than those with adequate health literacy (Sudore et al. 2006). This relationship was evident even after controlling for age, race, socioeconomic status, current health, health-care access and health-related behaviors.
Awareness about the importance of health literacy is growing. Proposed approaches to deal with the problem include evaluating public need, identifying obstacles to effective communication, increasing access and usability, and identifying communication and educational strategies appropriate to a targeted audience (Institute of Medicine 2004). To help specify educational strategies and interventions to improve the health literacy skills of older adults, research is presented on cognitive and motivational factors that support the acquisition of health information in later life. Knowledge acquisition is an important component of programs designed to increase health literacy.
Cognition and motivation
A wide array of basic cognitive abilities such as working memory, knowledge and language comprehension, as well as motivational factors, support health literacy and in particular the acquisition of new health information. Knowledge and motivation may be particularly important in later life due to developmental changes that occur in adulthood. Because of these changes, older adults may be more likely to conserve cognitive (Park et al. 1999) and emotional resources (Carstensen et al. 1999).
The acquisition of new health information is a function of basic cognitive skills such as working memory and language comprehension, as well as motivational factors.
Cognitive ability.
Cognitive changes in later life can be characterized in terms of the mechanics (the brain's hardware) and pragmatics (the brain's software) of intellectual functioning (Baltes 1987; Salthouse 2000). Aging is associated with declines in the mechanics of functioning, including areas such as executive function and working memory capacity. Working memory is used when individuals hold information in short-term memory while simultaneously performing a computation; for example, trying to understand a message left by your doctor's office on your answering machine, while at the same time writing down the telephone number that was spoken quickly during the first part of the message. Although working memory declines in later life, cognition models also acknowledge that aging is associated with gains in pragmatic intelligence, such as word meanings (vocabulary), general world knowledge, and domain-specific knowledge such as nutrition or one's chronic disease (Salthouse 2000; Schaie 1990).
Given the declines in one and preservation of the other, researchers have asked whether increases in knowledge and experience (pragmatics) can offset or compensate for losses in mechanics (Charness 2000). In support of this position, Miller et al. (2004) showed that older adults with high levels of knowledge were just as able as younger adults to learn about the heart in a 2-hour tutorial, and they were equally able to apply this new knowledge to understanding new passages about the heart as younger adults. However, other research has shown that age declines still remain within the highknowledge group. Relationships among performance, knowledge and age are complex, and there are several models that attempt to capture these relationships. According to the migration hypothesis, older adults sometimes migrate into higher knowledge groups, which in turn protects them from the declines experienced by older adults without this knowledge (Salthouse 2003).
This approach is promising because past work clearly shows that the amount of knowledge individuals possess regarding their health is closely tied to measures of health literacy as well as health outcomes (Dolan et al. 2004; Gazmararian et al. 2003; Kalichman et al. 2000; Williams et al. 1998; Wolf et al. 2005). Greater stores of health knowledge among older adults may protect against age declines in health literacy.
Language comprehension.
Language comprehension is an important component of health literacy. For example, individuals listen to and read information provided by health-care providers. They read label instructions to understand how to take medications properly and handouts regarding post-operative care. Individuals also listen to healthcare providers at clinics, reporters on the radio, pharmacists and others they encounter on a regular basis in order to make decisions regarding their health.
Language skills are also used to acquire new health information about a particular area. This can occur during brief communication exchanges with health-care providers as well as during more extensive searches on the Internet or at a library for information regarding chronic conditions or treatment options.
However, some aspects of language comprehension are compromised in later life due to age-related declines in working memory and related abilities (Norman et al. 1992; van der Linden et al. 1999). Language that is grammatically complex or packed with concepts is particularly difficult for older adults to comprehend (Wingfield and Stine-Morrow 2000). Indeed, some research shows that older adults have more difficulty understanding health information than younger adults (Brown and Park 2002).
Some aspects of language comprehension may be compromised in late life, making it more difficult to understand language that is grammatically complex or densely packed with ideas.
Researchers have examined ways to facilitate communication between providers and patients. Morrow et al. (2006) suggested that health materials should be presented in a way that reduces comprehension demands on general cognitive abilities as well as health literacy skills. Their work on medication adherence suggests that one way to achieve this goal is through patient-centered instructions, those written and organized in a way that is useful to the patient. In one study, for example, older adults preferred adherence information in the form of a schedule, and this preference was more pronounced among those with low health-literacy levels (Morrow et al. 2007).
Motivational factors.
One's ability to comprehend health information is critical for health literacy skills; one's willingness to do so is another matter. The extent to which individuals choose to engage in any particular health literacy endeavor, including comprehension, new knowledge acquisition and decision making, will depend on the cognitive resources available (ability) as well as the willingness or motivation to expend those resources. This notion is captured by prominent models of health behaviors (Bandura 2005; Leventhal and Mora 2005), which argue that motivational factors are necessary for compliance with what individuals may already know to be important behaviors.
Indeed, past research indicates that interventions focusing only on comprehension and knowledge acquisition do not always lead to changes. In nutrition, knowledge of healthy diets is not sufficient to encourage individuals to make healthy food choices (Nebeling et al. 2007). Motivation is also required.
Motivational factors underlying health literacy are not well understood, most likely due to problems surrounding their definition, operation and measurement. Nevertheless, measures have been developed to tap self-efficacy and control beliefs (those surrounding one's ability to attain desired goals) related to health outcomes (Wrosch et al. 2002) and eating behaviors (Moseley 1999). These beliefs may provide motivation for individuals to persevere when faced with health behaviors that are challenging, unpleasant or time consuming.
Such motivational forces have been widely researched in the area of cognition. For example, control beliefs and self-efficacy related to memory performance have been shown to be important for cognitive performance, particularly when the cognitive tasks are challenging (Bandura 1997). Within the aging literature, researchers have suggested that self-efficacy and control beliefs are particularly important for older adults because they lead to the more effective use of strategies, which in turn leads to higher levels of performance (Lachman and Andreoletti 2006; Miller and Lachman 1999). Older adults with a strong sense of control over their cognitive abilities allocated more attention to difficult reading passages than those with a weak sense of control (Miller and Gagne 2005). These data suggest that control beliefs may provide older adults with the motivation to persist in the face of a challenging comprehension task.
Although theoretical work suggests that self-beliefs are important for health (Bandura 2005), empirical evidence linking these beliefs to health comprehension and health outcomes is lacking. More research is needed to understand factors supporting the likelihood of adopting healthy behaviors as well as engaging the cognitive processes necessary to understand what those behaviors should be.
Prior knowledge and motivation
Health literacy represents a broad set of skills, one of which is the ability to comprehend health information so that new knowledge is acquired. The literature suggests that comprehension and learning in later life are dependent on cognitive and motivational factors. More specifically, prior knowledge and motivation may support learning by mitigating declines in processing mechanics (e.g., working memory) that are likely underlying comprehension difficulties. Therefore, prior knowledge and motivational factors are likely to be important for health comprehension and learning later in life.
We conducted two studies that examine the roles of knowledge and motivation on the acquisition of new health information. The specific question was whether knowledge and motivation mitigate age-related declines in learning about nutrition. In the first study, motivation specific to nutrition was assessed, whereas in the second study, motivation was assessed more broadly in terms of health. In both studies, the participants were high functioning, as reflected by years of education and scores on working memory measures.
Study 1.
In study 1, the sample included 30 younger (ages 18 to 35), 31 middle-aged (ages 36 to 59) and 32 older (ages 62 to 80) adults (data were from a larger study; Miller et al. 2010). Participants read two passages (1,400 words total) at their own pace and answered multiple-choice comprehension questions. The texts described the health benefits of consuming one of two types of foods (whole grains or fruits and vegetables) and provided information on how to identify these foods when selecting groceries.
Prior to reading the passages, participants completed a nutrition knowledge test and a battery of motivational measures. The knowledge test contained multiple-choice items (e.g., “A child who is raised on a vegan diet is most likely to become deficient in___”; options: fiber, carbohydrates, vitamin C, etc.). The nutrition motivation measure was a composite of three measures: the Food Pyramid Self-Efficacy Scale (Moseley 1999), a nutrition interest scale and a stage-of-change measure. The Food Pyramid Self-Efficacy Scale contained 22 items designed to assess individual perceptions of one's ability to follow a healthy diet when placed in a wide variety of circumstances, such as watching television or feeling restless or bored. The Nutrition Interest Scale consisted of six items (e.g., “How interested are you in knowing the difference between food facts and fallacies?”). The stage-of-change measure, modeled after Prochaska and DiClemente (1983), asked individuals to rate their readiness to follow a healthy diet within the areas of fruits and vegetables, fat and junk food. We created a composite measure of nutrition motivation by averaging the standardized scores across the three measures. Comprehension was assessed with a multiple-choice test.
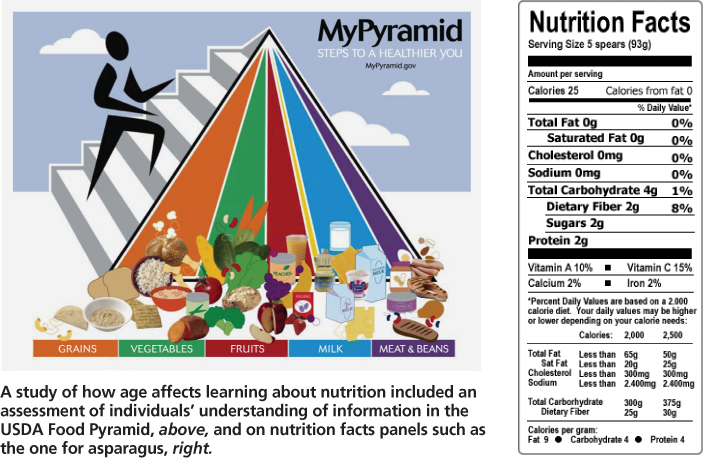
A study of how age affects learning about nutrition included an assessment of individuals’ understanding of information in the USDA Food Pyramid, above, and on nutrition facts panels such as the one for asparagus, right.
Consistent with past work on age differences in comprehension and recall (Johnson 2003), the results showed that comprehension performance significantly declined with age (r = −0.36, P < 0.001). However, there was a positive association between knowledge and age (r = 0.24, P < 0.05). Importantly, when knowledge was controlled, age differences in performance were magnified (r = −0.46, P < 0.001), indicating that without knowledge, older adults’ performance would have been even lower. A similar pattern was found for motivation. There was a positive age-trajectory in nutrition motivation (r = 0.34, P < 0.001), and larger age deficits in comprehension after controlling for motivation (r = −0.42, P < 0.001).
These findings are consistent with the migration hypothesis (Salthouse 2003), which suggests that adults migrate into higher levels of nutrition knowledge with increasing age, thereby mitigating further age-related declines in cognitive performance. These findings also extend the notion of migration to motivation by showing a similar age-related increase in self-efficacy and larger age differences in comprehension when self-efficacy is controlled. The implication of these findings is that knowledge and motivation related to nutrition play a larger role in later life by compensating for age-related declines in the mechanics of processing that underlie comprehension deficits.
Study 2.
The first study included a motivation assessment specific to nutrition, but motivation pertaining to more general health issues was not assessed. In study 2, the possibility that a more general measure of motivation mitigates comprehension declines was investigated. Data from this study, taken from a larger project (Miller and Gibson 2009), consisted of 102 adults between the ages of 18 and 81. Participants read a set of nutrition texts and completed several comprehension tasks. We focus on responses to a short-answer exercise completed after individuals read the texts (because it is most similar to the measure used in study 1) as well as the health motivation measure, Health-Engagement Control Strategies (HECS).
HECS was designed to assess the degree to which individuals engage in various strategies to control their health outcomes (Wrosch et al. 2002) and has been shown to be related to health outcomes (Wrosch and Schultz 2008). Participants responded to items such as, “I invest as much time and energy as possible to improve my health.” Knowledge was assessed using an expanded version of the nutrition test in study 1 (38 items). As with study 1, the goal was to determine whether knowledge and motivation mitigate age-related declines in comprehension performance.
The results were consistent with the first study, showing an age-related decline in comprehension performance (r = −0.30, P < 0.01), as well as a significant age-related increase in nutrition knowledge (r = 0.25, P < 0.01). Also consistent with the first study was the finding that age-related declines were more pronounced when nutrition knowledge was controlled (r = −0.46, P < 0.001). In addition, there was a positive correlation between age and health motivation (r = 0.44, P < 0.001), indicating that motivation to engage in strategies to control one's health increases with age. However, the correlation between health motivation and comprehension was nonsignificant (r = −0.11, P > 0.10). When motivation was controlled, age declines in comprehension performance were not magnified as in the first study; in fact, the correlation was slightly attenuated after controlling for motivation (r = −0.27, P < 0.01). These data fail to support the notion that health engagement strategies mitigate age-related declines in nutrition comprehension.
Research is needed to identify the motivational factors that promote engagement among seniors in education related to healthy behaviors, such as eating nutritious foods.
Nutrition comprehension and literacy
Together, data from the two studies show that nutrition knowledge mitigated age-related declines in nutrition comprehension, and that nutrition motivation also mitigated age-related declines. However, no mitigation was evident for the health motivation as assessed by HECS. Firm conclusions regarding which motivators do or do not provide additional support to older adults’ understanding of nutrition information are not possible without a wider range of measures within a single study to make direct comparisons.
Nonetheless, some speculations can be made. One possibility is that older adults who use more engagement strategies also have more health problems, which in turn offsets any potential benefits of increased motivation. Another possibility is that strategies used to control health behaviors are somewhat removed from one's motivation to learn about and follow a nutritious diet. Health motivation that is more specific may be more highly connected to behaviors than more general measures of health. This is the case when examining the relative effects of cognitive control beliefs and general control beliefs on cognitive performance; cognitive control beliefs are more highly connected to cognitive performance (Lachman 1986). Similarly, the benefits of nutrition motivation could be due to their overlap with nutrition knowledge. In examining the data, there was a significant positive correlation between nutrition knowledge and motivation in the first study (r = 0.23, P < 0.05). In contrast, the association between nutrition knowledge and health motivation in the second study was nonsignificant (r = 0.13, P > 0.10), indicating that individuals who reported using frequent strategies to control health outcomes were not necessarily those with greater stores of nutrition knowledge.
Although speculative, these findings could indicate that motivating factors within a health domain have greater effects on older adults when they are highly specific to that domain. The knowledge domain addressed here was nutrition; however, other specific health domains (e.g., glucose regulation, exercise) may show similar advantages.
Further questions
Although these findings shed some light on factors that support health literacy in later life, they also raise questions. One is, how does motivation support information acquisition and health literacy skills? Recent evidence suggests that nutrition motivation helps individuals sustain attention during a comprehension task (Miller et al. 2010). It could be that motivation within a domain provides individuals with the perseverance to engage in health literacy tasks that are cognitively demanding.
The samples in the two studies reported here were representative of high-functioning adults. Thus, the age effects reported here most likely represent a best-case scenario. It remains unclear how having fewer educational advantages would affect the opportunity for older adults to use knowledge and motivation to compensate for age-related declines in the mechanics of processing. Future research on health knowledge acquisition would benefit from a more diverse sample, which would help to determine if (1) motivational factors are constant across various educational or socioeconomic groups, and (2) patterns would be altered if age-related declines in comprehension were increased and knowledge levels were decreased, as may be expected within a less-educated group. Past research suggests that education would provide a substantial benefit for older adults (Wilson et al. 2009), but the mechanisms responsible for this are not well understood.
Increasing health literacy skills among older members of society is a goal that is growing in importance. A clearer understanding of factors that support health literacy in later life is essential if we are to meet the forthcoming demands on our health-care system and ultimately promote older adults’ quality of life. Research presented here suggests that prior knowledge plays a critical role in supporting the acquisition of new health knowledge, which in turn will support health literacy skills in later life. More effort should be directed toward educational programs to promote health behaviors among older adults.
The data also suggest that motivational factors support new knowledge acquisition and health literacy skills in later life. However, associations among knowledge, motivation and health literacy are complex. Greater effort should be directed toward research that identifies a wide range of motivational factors that encourage engagement in educational activities that promote healthy behaviors, such as eating healthy foods to prevent or control disease. To be sure, knowledge and motivation alone will not solve the problem of low health literacy or poor dietary habits. However, attention to these factors in addition to social marketing (e.g., encouraging manufacturers to reduce the number of foods processed with partially hydrogenated oils (trans fats), and identifying ways to provide affordable fresh fruits and vegetables to consumers in low-income urban areas) may provide an initial step toward increasing health literacy and improving health outcomes throughout adulthood.