All Issues
Emerging pathogens on the rise: How can waterborne illness be prevented?
Publication Information
California Agriculture 54(5):78-79. https://doi.org/10.3733/ca.v054n05p78
Published September 01, 2000
PDF | Citation | Permissions
Full text
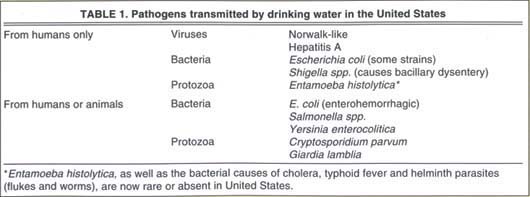
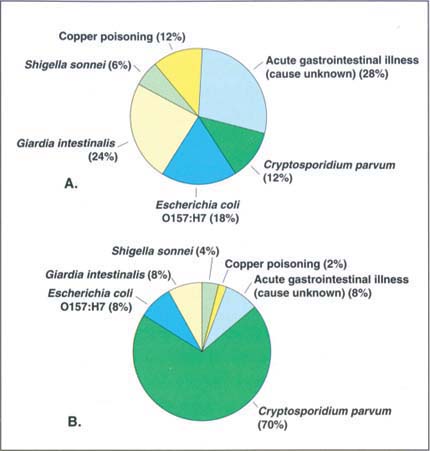
While historic microbes such as typhoid and cholera have been essentially eliminated from the U.S. drinking-water supply, new pathogens such as Cryptosporidium and Giardia have emerged as significant problems (table 1). Although most of the waterborne-illness cases reported by the U.S. Centers for Disease Control and Prevention (CDC) in 1997 and 1998 were associated with public water supplies, illnesses from private well water probably represent a greater proportion of the population served by such systems (Barwick et al. 2000) (fig. 1). (None of these outbreaks were reported from California.)
Except for Shigella sonnei and acute viral gastrointestinal illnesses, which are human-specific, the majority of the infectious agents causing outbreaks might have been of either human or animal origin. Public-health officials have placed a great deal of the onus for avoiding these hazards on largescale animal agriculture. However, as watershed management and nature protection grow in importance, scientists are also finding that feral animals can be sources of infectious agents in water.
Current federal policy by the U.S. Department of Agriculture and the Food and Drug Administration assumes that infectious agents such as Salmonella, E. coli O157:H7, and Campylobacter can be eliminated from farms; yet reservoirs of these agents in nature are common, and wild animals frequently visit farms to share the food and water with the domestic animals. Even Cryptosporidium parvum, whose presence in surface water is often blamed on cattle, has wild reservoirs such as feral swine (Atwill et al. 1997) and the California sea lion (Deng et al. 2000). Surface waters such as lakes and rivers that do not receive sewage are home to fish and birds, and ground-water from wells may contain dissolved substances (such as caffeine) or infectious agents. Sparkling clear mountain streams often contain cysts of Giardia intestinalis from resident beavers.
Outbreaks of waterborne disease occur because the water is inadequately treated or disinfected, or because it is recontaminated during distribution. Outbreaks are by no means limited to small communities or low-income areas; system failures can occur when the community does not obtain and maintain facilities adequately. Such problems include deterioration of source-water quality, obsolescent technology, inadequate upkeep of treatment and distribution facilities, and volume demands in excess of the system capacity ( see p. 69 ).
At the same time, certain segments of the population are especially vulnerable to waterborne illness due to advanced or young age, pregnancy or immunosuppression (CAST 1994); people at greater risk of waterborne illnesses may be better advised to boil their water than to drink from public supplies.
Emerging pathogens
Some disease agents are called “emerging pathogens” because they were unknown or not associated with water 10 or 20 years ago. Foremost among these is C. parvum, which caused 403,000 gastrointestinal illnesses (and contributed to about 100 deaths of AIDS patients) in the 1993 Milwaukee outbreak (MacKenzie et al. 1994), compared to less than 165,000 illnesses in all of the other drinking-water-associated outbreaks recorded in the United States between 1971 and 1998 (CDC 2000). While most emerging pathogens are not really new, they are being taken increasingly seriously as agents of waterborne disease. Treatments to remove or kill waterborne pathogens were devised and evaluated on the basis of their effects against bacteria. Viruses are harder to kill with disinfectants than are water-borne bacteria. Monitoring methods based on bacteria have not detected treatment failures such as that in the Milwaukee outbreak.
The CDC also reported two outbreaks of copper poisoning comprising 37 cases in 1997 and 1998 (fig. 1), both because of problems with the treatment and delivery of water that mobilized copper from pipes, rather than from copper contamination of the source water.
Essentially all of the infectious disease outbreaks reported to CDC resulted from deficiencies in treatment or disinfection; no illnesses from disinfection byproducts such as chlorination have been described. At present, no epidemiological data suggest that chlorinated drinking water increases the risk of cancer; risk from chlorine seems minimal, given the level or declining age-adjusted rates of all forms of cancer other than cancer of the lung and bronchus since 1930 (American Cancer Society 2000), while use of chlorine has increased.
Technological needs
Most U.S. residents distrust water that is even slightly turbid, with clearly visible suspended particles. Turbidity may indeed denote a hazard, as was learned during the 1993 outbreak of cryptosporidiosis in Milwaukee (MacKenzie et al. 1994). However, the notion that water that has been in a sewer can never be restored to safety and utility must be overcome (Vaux Jr. 2000). Waterborne pathogens are shed in feces by infected people. Wastewater has feces in it. If inadequately treated wastewater is used directly to produce drinking water, the risk of disease transmission is significant. Wastewater can be used safely in drinking-water production if several relatively costly technological safeguards are applied.
High-visibility water reuse is already being undertaken in some parts of California; moreover, a significant proportion of the water in the California aqueduct comprises effluents from upstream communities, destined to be reused with a minimum of ceremony or anxiety. UC researchers are addressing many aspects of water protection and safety, from containment of animal manure to discovery of little-known health effects associated with drinking water in long-term, special context studies (Cliver and Atwill 1997).
Water safety in 2025
The manner in which the water-treatment technologies are used to ensure safety is likely to be influenced by the hazard analysis and critical control point (HACCP) system, which was developed to safely feed the astronauts and is now widely used by the U.S. food industry (Stevenson and Bernard 1995). HACCP applies continuous monitoring at critical control points in a process to deal with anticipated hazards; current water treatment largely does the same, but often in a less organized fashion.
Water-distribution systems are infrastructure in the truest sense, since they are typically underground and out of sight; the political tendency to defer maintenance in such situations, especially in California, must be reversed. Alternately, the public may choose less stringent standards for publicly supplied water and adopt point-of-use treatment apparatus to do the final treatment (e.g., filtration through high-technology media) and disinfection (e.g., by ultraviolet light) of water that will actually be ingested. Point-of-use treatment requires careful maintenance at widely dispersed locations; additionally, low-income people may lack the resources to obtain the necessary technology. The final alternative is boiling water for drinking. The energy cost of this option is not extreme because of the small volumes involved, but boiled water is usually less flavorful and many people are unlikely to do this routinely and properly.
The future of safe drinking water in California in 2025 will depend on a great many factors. The projection of 48 million California residents by 2025 must be taken seriously. Great advances in the science and technology of water treatment and management will certainly occur in the coming decades. However, such advances can only be implemented if there is a collective will to do so and a commitment of significant public resources. The competing priorities of population growth, agriculture to grow food and fiber, and the will to preserve natural space and endangered species must be reconciled if we are to ensure safe and adequate water supplies while living on what is, metaphorically, a melting iceberg.
Fig. 1 Causes of (A) 17 outbreaks comprising (B) 2,038 illnesses from drinking water in the United States, 1997-1998. Source: Barwick et al. 2000.